
Did you know that over 1 million individuals worldwide undergo cardiac surgery via median sternotomy every year? (4)
In younger patients cardiac surgery is most commonly used to correct a congenital heart defect. In older patients surgery can be performed for various reasons such as; correcting a congenital heart defect, valve surgery, aorta repairs and frequently for coronary artery bypass graft surgery (CABGS) due to ischaemic heart disease.
To access the heart and cardiac vessels adequately a median sternotomy is performed. Following surgery the sternum is then usually wired to prevent movement while the sternum heals. Sternal stability can be achieved in the majority of individuals by 8-10 weeks without complications. (2)
In specific circumstances, cardiac surgery can also be performed via a Thoracotomy which is less invasive and can speed up recovery times. Thoracotomy patients can follow the same advice as for open chest surgery; however recovery time frames will most likely be faster than for a sternotomy.
Recovery from cardiac surgery can vary immensely from person to person and depends on many factors or events occurring pre, during or after surgery.
Looking after your sternum and moving again:
There are no specific evidence-based precautions or restrictions on arm movement and load following cardiac surgery. The majority of individuals can commence light upper limb mobility immediately after surgery, as instructed by your hospital staff.
Movement is encouraged for the following reasons;
- reduce sternal pain
- promote bone healing so it remodels in response to load
- keep your joints moving and healthy
- encourage good posture
- promote soft tissue healing
Initially movement will be without weight and in your pain free range.
Move in the Tube:
Several hospitals have taken up “move in the tube” as a functional and practical way to teach individuals how to safely move following a sternotomy (3, 4, 2) (Figure 1)
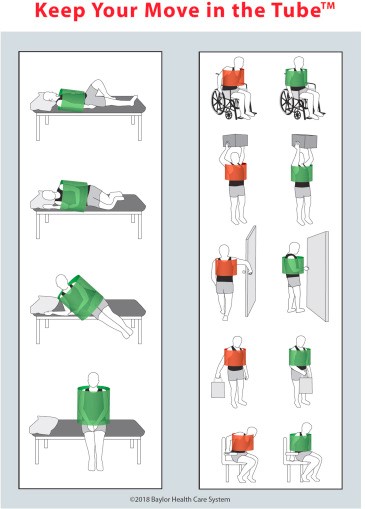
Figure 1 (3, 4)
Being nervous or anxious to move your upper limbs is very normal after sternotomy.
It is best to follow the direction and do the specific exercises you receive from hospital staff and your Cardiac Rehabilitation exercise specialists. (6)
Cardiac Rehabilitation can be commenced as early as 2 weeks after a sternotomy and is a vital step toward returning to your pre-surgical activities. (5)
If you have not been referred to Cardiac Rehabilitation, contact your local medical practitioner and discuss the options for a referral to a formal Cardiac Rehabilitation program locally.
Following surgery, participation in Cardiac Rehabilitation has been found to; increase functional capacity, improve cardiac risk factors, decrease symptoms and improve quality of life of individuals.
If you feel Cardiac Rehabilitation isn’t for you, consider having an initial assessment with your cardiac team to discuss your plan. They may offer a home exercise program, online or remote assistance. They will give you some direction on how to exercise safely at an early stage and also provide you with an avenue to ask questions if they arise, as you recover. (1, 7)
Returning to daily activities and rehabilitation exercise:
When you feel like getting back to daily activities which require lifting or commencing an exercise program, keep the following in mind:
- Start light
- Keep the weight close to your body to reduce the lever arm
- Avoid pushing and pulling early on
- Use both arms so the movement is symmetric. This loads both side of your sternum the same amount reducing stress on the healing bone
- Slowly reintroduce activities of daily living and recreational activities
- Exercise is best done under the guidance of an exercise specialist
- Movement with weight must be slow, controlled and progressive
- Weights can be progressively increased over your 12 week recovery period
- After 12 weeks you should be ready to start returning to your pre-surgical activities once cleared by your medical specialist
Seek advice if you are concerned about anything:
Complications following sternotomy can occur in 1%-8% of patients, so it is vital to discuss any concerns you may have in regards to your wound or sternal healing, with your health care specialist or cardiac rehabilitation team (3, 4), and also always attend your follow-up appointments.

Remember to monitor yourself and STOP and seek medical help if you notice similar symptoms that you experiences prior to your surgery.
Fatigue:
Feeling fatigued is common following cardiac surgery.
Not only do you need to go slowly to allow sternal recovery, it is important to listen to your body and consider levels of fatigue when starting a recovery program.
However don’t let fatigue stop you from becoming more active. Small amounts of activity will assist you to recover and you will slowly start feeling less fatigued.
Walking:
Along with specific individualised and progressive upper limb exercises for sternal recovery, your recovery will be complemented by commencing light aerobic exercise like walking.
Start with walking slowly for a short period of time, gradually increase duration first and then intensity as tolerable. Each stage can be as long or as short as you need it to be before you progress to the next.
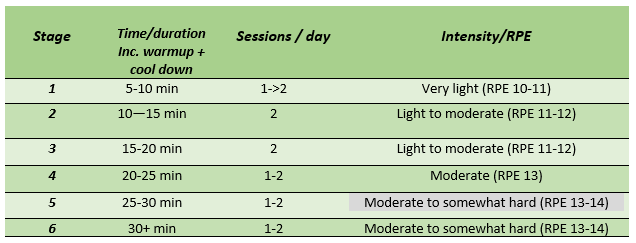
Refer to table below as a guide to returning to walking.
Progressive walking guide following Cardiac Surgery
If 30 minutes is too much in one session, break it up. For example: 3×10 min sessions
Intensity:
Intensity is the key! Always start at a light intensity.
You will know it’s the correct intensity if you feel comfortable the whole time during the exercise, you can still have a conversation.
You should also be able to recover well immediately after and also continue to feel good the following day. Initially take on a little less than you think you can to avoid over doing it.
One stage may last 1-2 or even 3 weeks depending on individual factors.
A good tool to use is the BORG RPE scale (Rating of your perceived exertion).
This means that you rate how heavy or strenuous the exercise feels to you, using muscular strain and breathlessness as your guide.
The recommended starting intensity for exercise is around PRE 11-12.
Over time you will start feeling fitter, stronger and less fatigued. When you feel ready, you may be able to gradually increase intensity to 11-14 RPE range (Figure 3)
BORG RPE SCALE: Rating of Perceived Exertion

Goal setting:
Once you have been discharged from hospital, your sights will be set on recovery and returning to your pre-surgical activities.
If you have not received an activity guide or a personalised activity plan, speak to your Cardiac Rehabilitation team, Medical Specialist or Exercise Physiologist to make a plan.
Your plan may include short and long term goals to help you resume your pre-surgical activities at the appropriate stage of recovery consistent with your individual health situation. (8)
| Example of how a return to activities plan might look like for golf ; (This is an example only. Always speak to your exercise or cardiac specialist before returning to any sport) Week 2-4 walk daily and start cardiac rehab Week 4-6 cardiac rehab exercises and walking Week 6-8 light putting and light half swing without a club in your hands (simulation) Week 8-10 light chipping and normal putting. ¾ to full swing without a club in your hands (simulation only, work on stance, technique etc) Week 10-12 slow half swing with a light club – progress to ¾ swing with a light club. Hit the ball with light force only or don’t hit the ball just yet Week 12+ start with light/slow drive then progressively building up to all other shots over several weeks to a few months depending on the individual. |
The importance of exercise following cardiac surgery:
Your whole body will benefit not just your heart!
- improves muscular strength
- reduces post-surgical fatigue
- can help lower blood pressure
- increases bone density
- improves exercise capacity and overall energy levels
- strengthens immune system
- decreases the risk of heart disease
- helps control/reduce body weight
- improves mood/mental health
- improve quality of life
Did you have a heart attack prior to surgery?
If you have had surgery following a heart attack there is more information specific to heart attacks here.
References:
- A.C.P.I.C.P Standards (2015) Standards for Physical Activity and Exercise in the Cardiovascular Population, 3rd Edition pp.43-45 [online] Available at; https://www.acpicr.com/data/Page_Downloads/ACPICRStandards.pdf
- ACSM (2022) ‘Guidelines for exercise testing and prescription’ (11th edition), Wolters Kluwer, p240-241
- Adams J et al, ‘An alternative approach to prescribing sternal precautions after median sternotomy, “Keep Your Move In The Tube”, Baylor University Medical Centre Proceedings, 2016; Vol 29 (No 1) p97-100
- El-Ansary D et al, ‘An evidence-Based Perspective on movement and Activity following Median Sternotomy,’Physical Therapy Dec 2019, Vol 99, Number 12 p1587-1601 [online] Available from; https://academic.oup.com/ptj/article/99/12/1587/5558221
- Ennis S et al (2022) ‘Effectiveness and Safety of Early Initiation of Post sternotomy Cardiac Rehabilitation Exercise Training’, JAMA Cardiol 2022 Aug 1; 7(8):817-824. [online] Available from: doi;10.1001/jamacardio.2022.1651
- Katijjahbr MA et al (2018) ‘Standard restrictive sternal precautions and modified sternal precautions had similar effects in people after cardiac surgery via median sternotomy (SMART Trial): a randomised trial, Journal of Physiotherapy, Vol 64,p97-106
- Marwick T et al, Barker Heat & Diabetes Institute Report, ‘No Second Chances, Controlling Risk in Cardiovascular disease’ p44-45 [online]; Available at; https://baker.edu.au/impact/advocacy/no-second-chances
- Parker R, Adams J, (2008) “Activity Restrictions and recovery after open chest surgery: understanding the patient’s perspective”, Baylor University Medical Centre Proceedings, Vol 21 (No 4) p421-425
